Causes of the disease
Impaired blood flow occurs against the background of various factors and conditions. The result of poor vascular function will be the appearance of areas of hypoxia in the initial stages and leukoaraiosis or areas of liquefaction in the later stages. At first, the lesions are characterized by small size and sparseness in different parts of the brain, which leads to a variety of symptoms.
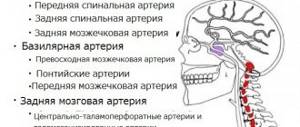
Lesions are most often localized in the area of two vascular beds:
- carotid artery;
- vertebrobasilar artery.
At the early stage of dyscirculatory encephalopathy, the nervous system tries to compensate for lost functions by creating other neural connections. Over time, compensation is lost or oxygen starvation occurs in previously functioning areas. At a late stage of pathology, a person faces disability. The consequence of dyscirculatory encephalopathy is the death of parts of the brain, which makes the pathological condition reminiscent of a stroke. However, the process occurs over years; neurological deficits accumulate over a long period of time and do not arise suddenly as a result of an acute disturbance of blood flow.
There are many diseases and conditions that can reduce the lumen of the arteries that supply blood to the brain. But most often, vascular encephalopathy of the brain develops against the background of:
- Atherosclerosis of blood vessels due to the deposition of lipids on the internal walls as a result of damage to the endothelium and impaired fat metabolism.
- Progressive malignant hypertension, in which blood pressure increases abruptly, which affects cerebral perfusion pressure and brain nutrition. As a result, the vessels begin to leak blood directly into the tissue, which leads to a protective spasm in a certain area and disruption of blood supply. With vascular encephalopathy, hypertension develops against the background of polycystic disease, chronic kidney inflammation, adrenal tumors, and Cushing's syndrome.
Other causes of dyscirculatory encephalopathy include:
- Narrowing of the vertebral arteries leads to a decrease in the vertebrobasilar region with osteochondrosis, muscle spasms, injuries, dysplasia, pathology of the first cervical vertebra (Kimerli anomaly) and malformations of the artery itself.
- Frequent and sudden drops in blood pressure impair cerebral perfusion pressure.
- Autoimmune inflammatory processes in blood vessels.
- Diabetes mellitus causes vascular restructuring and problems with blood supply.
- Arrhythmias of various types are associated with a decrease in blood output and the appearance of a deficiency in brain nutrition.
- Hereditary vascular anomalies.
- Alcoholism and smoking.
- Endocrine abnormalities that cause narrowing or dilatation of the arteries.
- Thrombosis of cerebral arteries and veins.
The mechanism of development of the pathology determines several types of dyscirculatory encephalopathy:
- Atherosclerotic - almost 50% of all cases.
- Hypertensive - approximately 48% of diseases.
- Venous - against the background of tumors, pulmonary and heart failure.
- Mixed - a combination of atherosclerotic lesions and hypertension.
The causes of vascular dysfunction are different, but the consequences are the same. Impaired blood flow leads to the gradual development of neurological deficits.
The pace and dynamics of the development of the disease allows us to highlight:
- Fast (2 years per stage) and slow (5 years per stage) progression.
- A remitting form with a gradual increase in symptoms, the onset of temporary clarity of consciousness, but a constant decrease in cognitive functions.
- The classic course is associated with a slow and long-term development of symptoms with the progression of dementia.
Diagnosis of discirculatory encephalopathy: essence
Lack of oxygen and nutrients against the background of stenosis of the main arteries and veins after a certain period provokes disruption of the functioning of brain cells. Diffuse tissue damage negatively affects the speed of reactions, psycho-emotional state, motor, mental, and physical activity.
You should consult a neurologist if you have frequent headaches, memory loss, insomnia, or vestibular disorders. Consultation with a specialist is needed if problems arise with the perception and processing of information, emotional instability develops, coordination is reduced, gait has changed, and dizziness and nausea occur when walking.
Encephalopathy on MRI
Early diagnosis and timely initiation of treatment for dyscirculatory encephalopathy (DEP) prevents severe neurological disorders and reduces the risk of impairment of mental and cognitive functions.
Inattention to the manifestations of pathology against the background of diffuse brain damage leads to increased disorders of the emotional-volitional sphere, problems with motor activity, performance, memory, vision, and hearing.
Clinical picture
Signs of dyscirculatory encephalopathy depend on the degree of damage to a particular area of the brain, but the main neurological abnormalities include:
- personality disorders: tearfulness, suspiciousness, aggression and irritability, change in character;
- problems with understanding and reproducing speech;
- impairment of memory and knowledge formation, inability to transmit and comprehend information;
- deficiency of hearing, smell, vision;
- pain in the temples and occipital region, pressure in the eyes, nausea and vomiting;
- problems with the vestibular system: dizziness, staggering, poor coordination, tinnitus;
- insomnia, interrupted sleep and drowsiness;
- autonomic dysfunctions: vomiting, nausea, sweating, dry mouth;
- mood swings, depression, tearfulness.
The severity of symptoms depends on the stage of the disease.
Discirculatory encephalopathy of the 1st degree is characterized by emotional disturbances, which in older people are usually associated with age. A manifestation of pathology can be depression, which comes with attacks of apathy and hypochondria in the absence of problems at home and at work.
Emotional manifestations affect health. The person complains of pain in the back, head, and leg joints, but not of depression and sudden mood swings from naive childish joy to crying and an aggressive attitude towards loved ones. People complain of sleep problems, fatigue, headaches and absent-mindedness. However, all emotional manifestations are combined with a decrease in cognitive function. Early manifestations of impaired brain function include:
- inability to concentrate;
- bad memory;
- fatigue during mental work.
A person becomes disorganized, cannot plan his own time, loses commitment, forgets events from the past, and gets lost in information he heard recently. The gait becomes unsteady, coordination of movements worsens. While walking, you may feel dizzy and feel nauseous.
The diagnosis of dyscirculatory encephalopathy of the 2nd degree is made when symptoms intensify, a marked decrease in intelligence, thinking and memory. The patient is able to assess his own condition, but exaggerates the possibilities. At this stage, a person has to quit his job or move to his family due to everyday difficulties. Apathy covers him most of the time, the patient sits idle for hours, becomes indifferent to everything that previously interested him. Memory problems are increasing, and his family should be aware that he can get lost, even if he goes out to the next store. Emotional alienation and indifference to loved ones are growing. The gait becomes shuffling.
Discirculatory encephalopathy grade 3. With this form, cognitive functions and the ability to act purposefully are completely lost. The emotional, spatial and temporal connection with the outside world is lost. A person cannot speak; automatisms appear in speech. Movements are impaired to the point of paresis, and convulsive attacks occur. The functions of urination and defecation are not controlled. A stage develops when any movement of the patient can lead to a fall. Life passes in a sitting or lying position, self-care skills are lost: the patient needs to be fed, dressed, and provided with hygienic care. At the last stage, discirculatory encephalopathy symptoms transform into dementia: the difficulties of emotional disorders associated with sharp anger, arguments and the need to seek verbal contact disappear.
Forecasts
Most often, adequate and systematic treatment of the disease can significantly slow down the development of dyscirculatory encephalopathy, but this only applies to the first and second stages. Sometimes a rapidly progressing pathology is observed, in which the next stage occurs two years after the start of the previous one.
An unfavorable prognosis is usually given if dyscirculatory encephalopathy is combined with degenerative changes in the brain. The situation is also complicated by acute cerebral circulatory disorders, hypertensive crises, and poorly controlled hyperglycemia.
Recognize and prevent
Relatives of patients dying from strokes, heart attacks, or pulmonary edema have no idea what vascular encephalopathy is and how the pathology affected the emotional state of the relative.
Early signs are usually overlooked. But a visit to a neurologist for a person with hypertension, diabetes and atherosclerosis is mandatory. Simple cognitive tests can reveal a disorder and become a reason for a comprehensive diagnosis with an examination by an ophthalmologist. Ultrasound of the vessels of the head and neck helps to suspect pathology. Standards for the treatment of dyscirculatory encephalopathy require a full range of examinations by a vascular surgeon, endocrinologist and cardiologist.
To prevent dementia, it is necessary to eliminate the disease that impairs vascular function. This is followed by a set of measures related to the prevention of strokes.
At the early stage of dyscirculatory encephalopathy and to reduce the risk of its development, it is recommended:
- Normalize body weight.
- Improve the quality and composition of food.
- To refuse from bad habits.
- Add physical activity.
Excess weight and a sedentary lifestyle are risk factors for atherosclerosis, type 2 diabetes and hypertension. Without lifestyle adjustments and efforts on the part of the patient, the risk of vascular disorders cannot be overcome.
Nutrition involves avoiding fatty meats, canned fats, baked goods and sweets to lose weight and clear arteries. The diet is filled with vitamins, healthy fats, and seafood.
You need to walk thirty minutes a day, do light exercises, and keep your muscles toned. The condition of blood vessels and the heart directly depends on physical activity.
Operation
Indications for surgical treatment:
- severe damage to important main arteries in the head area;
- occlusion or narrowing of more than 2/3 of the lumen of the vessel;
- active increase in cognitive impairment and neurological signs;
- critical narrowing of the arteries due to a microstroke.
Types of surgical intervention in the internal carotid artery:
- extra-intracranial microanastomosis is performed with complete occlusion;
- endarterectomy is prescribed for severe stenosis.
The last degree of brain encephalopathy - grade 3 dyscirculatory encephalopathy - is the most severe. In some cases, death occurs, but supportive treatment is possible.
You can read more information about dyscirculatory encephalopathy and its symptoms in this publication.
Treatment with drugs
Drug treatment for dyscirculatory encephalopathy is comprehensive as it targets hypertension, poor lipid profile, high blood sugar and excess weight:
- Angiotensin-converting enzyme inhibitors normalize not only blood pressure, but also cholesterol and glucose levels, improve blood supply to the heart muscle and slow the progression of hypertrophy, and are used in the prevention of strokes. The drugs are prescribed for heart failure, metabolic syndrome, and significantly reduce the risk of brain damage.
- Beta-blockers are prescribed for hypertension, coronary heart disease, angina pectoris, arrhythmias, and prevent vasospasm and excess load on the arteries and heart.
- Calcium channel antagonists relax vascular smooth muscle cells, reduce cardiac ischemia, and improve blood circulation. Studies have shown that Nimodipine helps restore cognitive function in older people.
- Diuretics remove excess fluid, affecting the volume of circulating blood. Most often they are used in combination with other antihypertensive drugs.
Drug therapy should affect the risk of atherosclerosis and improve lipid metabolism. The most popular drugs are derivatives of nicotinic and fibric acids, as well as statins, which directly regulate the production of cholesterol in the body. Fatty acid sequestrants, fish oil, and vitamins C and E are also used.
Dyscirculatory encephalopathy during treatment must be controlled symptomatically, which is facilitated by drugs acting on microcirculation, sedatives and tranquilizers to alleviate emotional dysfunctions.
Substances that directly dilate them help improve the functioning of blood vessels. They are prescribed for a diagnosed decrease in blood flow in the carotid artery, improve blood flow in the capillaries, relieve headaches, and correct cognitive function. To improve venous outflow, medications are prescribed to increase tone and improve capillary permeability (“Vasobral”).
Nootropic drugs and neuroprotectors affect metabolic processes in nerve tissues, protect neurons during hypoxia, reducing oxidative stress and the risk of blood clots. Taking these medications prevents vasospasm, and therefore generally affects cognitive health. The effect appears only after a month, so intravenous infusions are usually prescribed.
Additionally, blood clotting regulators (Cardiomagnyl) are used.
Relatives of patients are often concerned about how long they can live with grade 3 dyscirculatory encephalopathy. However, with irreversible changes in the brain, one should not expect a significant improvement in the condition. Prognosis depends on the nature of the disease, which is determined in the early stages and depends on the control of concomitant diseases.